Stages of Rabies Infection and Treatment Options Following Animal Bite
Stage 1: Virus Entry and Local Replication
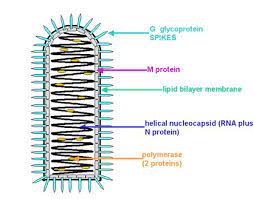
In the context of a rabies infection initiated by an encounter with an infected animal, the initial stage unveils a sequence of events that are crucial to understanding the pathogenesis. As the animal’s incisive bite punctures the skin, it acts as a vector for the rabies virus harbored within its saliva. This virus, a neurotropic agent, exploits this entry point to gain access to the host’s internal milieu. The virus takes advantage of the disrupted tissue integrity to infiltrate local cells, predominantly those in proximity to the bite site. These cells serve as an unwitting factory, where the virus undergoes replication, capitalizing on the host’s cellular machinery to amplify its population. This stage marks the initiation of an intricate biological process, where the virus’s genetic material drives the production of virions, ready to perpetuate the infection.

This localized replication sets the foundation for subsequent stages, as the virus accumulates and spreads, progressively establishing a foothold on the host’s physiology. This initial phase, characterized by viral replication at the site of entry, represents a critical juncture in the timeline of rabies infection, laying the groundwork for the virus’s subsequent journey along the neural pathways toward the central nervous system.
Stage 2: Peripheral Nervous System Infection
Upon completing its initial replication at the bite site, the rabies virus embarks on an intricate journey orchestrated by its neurotropic predilection. Exploiting the peripheral nervous system’s intricate network, the virus initiates its infiltration of peripheral nerves, which extend beyond the confines of the brain and spinal cord. This phase of the infection, characterized by the virus’s propagation along these nerve fibers, serves as a pivotal conduit for the virus to reach its ultimate destination – the central nervous system (CNS). Central to this progression is the phenomenon of retrograde axonal transport, a process in which the virus capitalizes on the neuronal machinery to move in a reverse direction along the nerve fibers. This methodical mode of travel underscores the virus’s adeptness at co-opting the host’s cellular mechanisms for its own propagation. The virus exploits the microtubule-based transport system within neurons, effectively allowing it to journey along the nerve fibers towards the cell body.
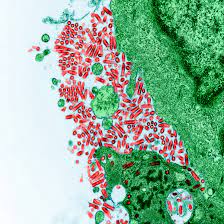
As the virus traverses these peripheral nerves, localized sensory manifestations may become evident. Notably, the bite site itself becomes a locus of sensory disturbance, often evoking sensations of pain, tingling, or itching. This sensory aberration, attributable to the virus’s interference with the peripheral sensory neurons, serves as an early indication of the virus’s insidious infiltration. It stands as a testament to the virus’s capacity to manipulate the intricate neural pathways and perturb the host’s physiological equilibrium. The culmination of this stage is the virus’s relentless advancement towards the central nervous system, setting the stage for the subsequent phases of the infection’s progression. This intricate interplay between viral propagation, retrograde axonal transport, and localized sensory perturbations underscores the virus’s capacity to subvert the host’s neural architecture, reshaping its trajectory in a manner both ominous and scientifically intriguing.
Stage 3: Central Nervous System Infection

CNS Invasion and the Onset of Prodromal Phase
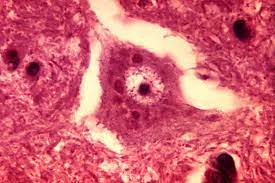
With the culmination of its pernicious journey along the peripheral nervous system, the rabies virus, driven by its neurotropic predilection, surmounts the final frontier – the impenetrable bastion of the central nervous system (CNS). This pivotal juncture heralds the virus’s infiltration into the sanctum of the brain and spinal cord, where its sinister machinations take root. Central to this stage is the virus’s ability to breach the formidable barriers guarding the CNS. As the virus invades the neural tissue, it capitalizes on cellular receptors within the CNS to facilitate its entry. This meticulous process underscores the virus’s aptitude for manipulating host cellular machinery to its advantage, enabling its insidious dissemination within the hallowed confines of the CNS.
Following this CNS invasion, a distinct phase known as the prodromal phase unfolds. During this incipient period, the host’s immune response is engaged in a delicate dance with the intruding virus. Initial symptoms begin to emerge, reflective of the virus’s impact on the host’s homeostatic equilibrium. Fever, headache, and general malaise typify this phase, representing the immune system’s initial recognition of the viral intrusion and its efforts to mount a response. These prodromal symptoms, while seemingly non-specific, are emblematic of the virus’s systemic impact and the host’s incipient struggle against its encroachment. The virus’s establishment within the CNS precipitates an array of physiological disturbances, heralding the subsequent phases that herald a cascade of neurological manifestations, leading ultimately to the harrowing clinical expression of rabies. As the prodromal phase unfurls, the intricate interplay between viral invasion, immune response, and the host’s physiological reactions sets the stage for the subsequent stages of rabies pathogenesis. This nuanced interplay stands as a testament to the virus’s capacity to manipulate the host’s intricate neural architecture and to the intricate choreography of immunological defense against this formidable adversary.
Stage 4: Clinical Rabies
The Dual Phases of Clinical Manifestations
The clinical phase of rabies infection ushers in a series of neurological and physiological manifestations that underscore the virus’s profound impact on the host’s central nervous system. This stage is characterized by a bifurcated progression, featuring two distinct phases – the excitative phase followed by the paralytic phase.
Excitative Phase: A Glimpse into Neuropsychiatric Turmoil. The excitative phase unveils a startling range of neuropsychiatric disruptions, highlighting the virus’s profound impact on the intricate neural networks that oversee cognition and emotion. Throughout this phase, the virus’s presence within the limbic system triggers a variety of symptoms that evoke an innate sense of apprehension. Anxiety, confusion, agitation, and hallucinations cast an unsettling veil over the individual affected. The virus manipulates the intricate structure of the limbic system to induce emotional volatility and cognitive confusion. This phase provides a chilling insight into the virus’s capacity to exert transformative effects on an individual’s mental state.
Paralytic Phase: Descending into Motor Dysfunction. Running parallel to the excitative phase, the paralytic phase unravels, revealing a progression characterized by compromised muscles and motor dysfunction. Muscle weakness and paralysis become increasingly dominant, extending their insidious hold throughout the host’s body. Swallowing turns arduous as throat muscles undergo spastic contractions, triggering the hallmark hydrophobia symptom—an irrational fear of water due to the excruciating pain experienced while attempting to swallow. Moreover, the paralytic phase induces aerophobia, where the host grapples with breathing. This suffocating ordeal results from compromised respiratory muscles, leading to distressing respiratory insufficiency. The very act of breathing becomes a daunting struggle, a poignant reflection of the virus’s systemic intrusion. The excitative and paralytic phases present compelling illustrations of the virus’s intricate interaction with the host’s neural and muscular systems. These phases unfold with a chilling relentlessness, tracing the virus’s impact as it navigates through the intricate matrix of the central nervous system. Ultimately, they underscore the clinical severity of rabies infection.

Stage 5: Coma and Death
The Unfolding of Terminal Stages
As the inexorable trajectory of the rabies infection reaches its terminal juncture, the host’s physiology succumbs to the implacable dominance of the virus. This final stage encapsulates the grim culmination of the virus’s relentless assault on the central nervous system and the resultant consequences that ensue.
Coma: As the infection progresses, a shroud of uncertainty envelops the individual’s consciousness. The once-cohesive symphony of brain activity descends into disarray, a consequence of the virus’s forceful assault on the brain’s intricate connections. This disruption culminates in profound neurological dysfunction, ushering in a coma – a somber state where cognitive faculties are submerged. Within this coma phase, cogitation and perception are veiled by a profound stillness, accentuating a significant deterioration in brain function. The virus’s relentless propagation across the central nervous system underscores its potency in disturbing conscious awareness, propelling the person into a realm of detached slumber.
Death: As the infection reaches its ultimate stages, the culmination of symptoms ushers in an inescapable outcome – death. In instances of clinical rabies, the grim reality of death is regrettably highly probable. This stems from the virus’s sweeping assault on crucial functions, particularly those intertwined with respiration. Respiratory failure, a dire consequence of the virus’s influence on the systems accountable for breathing, emerges as the primary cause of death. The transition towards death usually transpires within a span of days to weeks from the onset of symptoms, as the virus’s dominance over neural, muscular, and systemic processes overrides the body’s defenses. The individual’s battle against rabies concludes on a sorrowful note, laying bare the virus’s mastery over the delicate equilibrium of the central nervous system and the interconnected systems it oversees.
When you find yourself facing the unsettling possibility of contracting rabies due to an animal bite, a glimmer of hope emerges in the form of post-exposure prophylaxis (PEP). This treatment offers a potential remedy, provided you initiate it before symptoms manifest. Picture this: an animal that could potentially carry rabies has bitten you – it is an unsettling thought. But post-exposure prophylaxis (PEP) that might come to your aid. It acts as a specialized treatment that could mitigate the severity of the illness, though it is not foolproof. The key with PEP is to begin it before you start experiencing symptoms.
PEP serves as a beacon of optimism when concerns about rabies arise. It offers a means to access medical assistance immediately after a bite from a potentially infected animal. The concept is to impede the virus’s progression before it gains a foothold in your body. By undergoing treatment before signs of sickness appear, it is akin to halting the virus in its tracks before it disrupts your nervous system and triggers those distressing symptoms.
PEP holds significant importance because it holds the potential to spare you from severe illness due to rabies. It serves as a reminder that acting swiftly and remaining vigilant after an animal bite can provide you with an opportunity to safeguard your well-being. It is important to intercept the virus before it gains excessive strength and inflicts substantial harm.

Treatment Options:
Wound Cleaning: Mitigating the Risk
Following a bite, promptly cleaning the wound with soap and water emerges as a pivotal step. This action serves to wash away a portion of the virus, diminishing the potential for its dissemination within the body. Swift initiation is pivotal in impeding the virus’s establishment.
Administration of Rabies Immune Globulin (RIG): Augmenting Protection
Medical professionals might administer rabies immune globulin (RIG) proximate to the bite site. This substance acts akin to a protective barrier, furnishing immediate defense against the virus. It facilitates an accelerated immune system response in case the virus is present.
Rabies Vaccination: Fortifying Immunity
A series of rabies vaccine injections will also be needed over several weeks. This vaccination regimen equips your body with the means to combat the rabies virus. The shots play a crucial role in instructing your immune system to identify and neutralize the virus’s threat if it endeavors to induce illness.
Final Conclusion
Hence, through wound cleaning, RIG administration, and rabies vaccination, you are offering yourself a strong chance to halt the virus’s harmful effects. It is all about quick action and providing your body with the necessary tools to combat the virus before it worsens.
When faced with the potentially life-threatening threat of rabies infection, seeking immediate medical care becomes an imperative of paramount importance. The harsh reality of rabies is its swift progression from exposure to clinical symptoms, leaving minimal room for hesitation. Timely medical attention post an animal bite, especially one involving potential rabies exposure, can be the deciding factor between life and dire consequences.
The stages of rabies infection unfold rapidly, leading to irreversible neurological harm and, eventually, death. Yet, there exists a critical opportunity – a short span after exposure – during which swift medical intervention can prevent the virus from establishing a foothold. Post-exposure prophylaxis (PEP) presents a lifeline, comprising wound cleaning, rabies immune globulin (RIG), and a series of vaccines.
Taking prompt action to clean the wound, receive RIG, and initiate the vaccine regimen empowers the body to mount a defense against the encroaching virus. This proactive approach bolsters the immune system’s arsenal, enabling it to thwart the infection’s advancement before it evolves into an unmanageable medical emergency.
Remember, the urgency of seeking immediate medical attention is A MUST. Time is crucial in the fight against rabies, and every passing moment could lead to dire outcomes. By prioritizing swift medical care after a potential rabies exposure, you are taking a pivotal step to safeguard your health and well-being, ensuring that the threat of rabies infection remains under control.






